Hospital Psychology: Healing Beyond the Medical Chart
When serious illness strikes, the body isn’t the only thing that needs care. Fear, uncertainty, grief, isolation, loss of control—these emotional realities accompany every patient who enters a hospital, yet medical treatment alone rarely addresses them. This is where hospital psychology becomes essential, transforming clinical spaces into environments that recognize patients as whole human beings rather than collections of symptoms to be managed.
Hospital psychologists work at the intersection of physical and emotional health, understanding that addressing psychological needs isn’t a luxury but a fundamental component of effective healthcare. This article explores what hospital psychologists do, why their presence matters so profoundly, and how they contribute to more humane medical care.
What Hospital Psychology Encompasses
Hospital psychology represents a specialized branch of psychology practiced within healthcare settings—hospitals, clinics, rehabilitation centers, and other medical environments. These psychologists work alongside physicians, nurses, and other healthcare providers to address the psychological dimensions of illness, injury, and medical treatment.
Their work recognizes a truth that medical systems sometimes overlook: illness is never purely physical. A cancer diagnosis doesn’t just affect cells—it triggers existential questions, threatens identity, strains relationships, and can shake someone’s entire sense of reality. A traumatic injury doesn’t just damage the body—it can shatter assumptions about safety and control. Chronic illness doesn’t just require medication management—it demands psychological adaptation to an altered life.
Hospital psychologists practice across diverse medical settings, each with distinct psychological challenges. In oncology units, they support patients facing cancer’s profound uncertainties. In pediatric wards, they help children cope with frightening experiences and lengthy hospitalizations. In intensive care units, they assist families making impossible decisions and patients recovering from life-threatening crises. In palliative care, they help people find meaning and peace as life draws to a close. In maternity wards, they address perinatal mental health. In transplant units, they support patients through the psychological complexity of receiving life-saving organs.
This presence throughout the hospital reflects an understanding that psychological needs arise wherever medicine is practiced.
The Hospital Psychologist’s Essential Functions
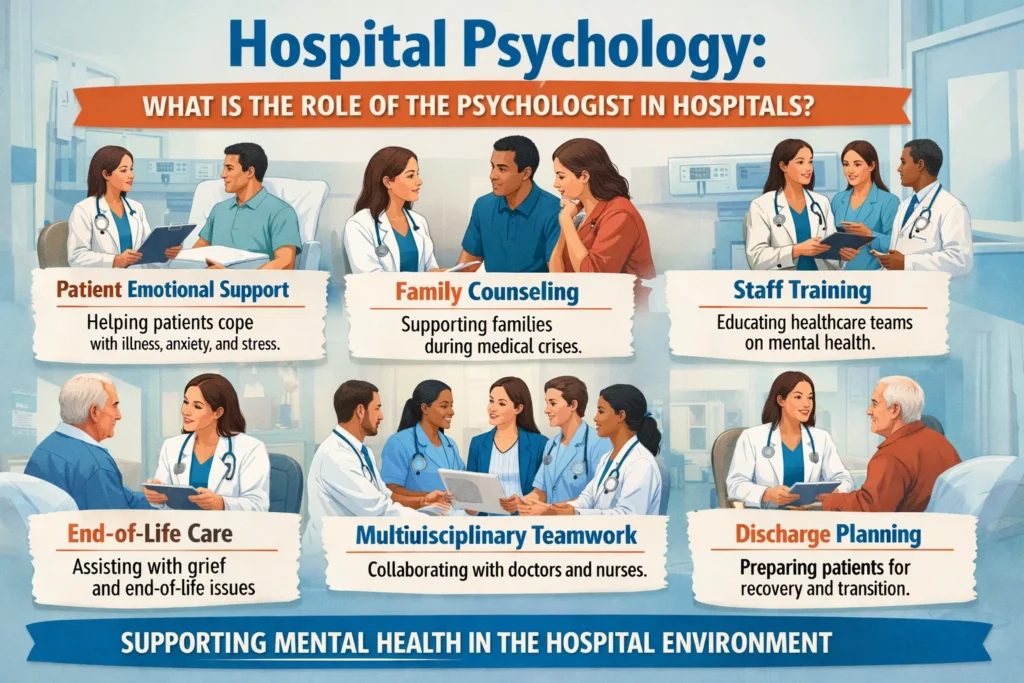
Hospital psychologists serve multiple crucial roles, adapting their work to each patient’s unique circumstances while addressing common psychological challenges that accompany medical treatment.
Providing emotional support during crisis: Hospitalization itself creates stress, even before considering the underlying illness. Patients lose autonomy, privacy, and normal routines. They face painful procedures, uncertain prognoses, and separation from loved ones. They navigate confusing medical systems while often feeling physically terrible. Hospital psychologists offer patients space to express the fear, anger, sadness, and frustration that naturally arise, validating these emotions rather than dismissing them as obstacles to medical care.
Facilitating adaptation: Adjusting to illness, treatment demands, and hospital environments requires psychological work. A psychologist might help someone newly diagnosed with diabetes process this identity shift and develop strategies for managing the condition long-term. They might assist a trauma patient in comprehending what happened and what recovery will require. They help patients develop realistic expectations, identify coping resources, and find ways to maintain some sense of control amid circumstances that feel overwhelming.
Supporting families: Illness affects entire family systems. Parents watching their child suffer experience their own trauma. Adult children making medical decisions for aging parents face guilt and grief. Spouses become caregivers, fundamentally altering relationship dynamics. Hospital psychologists help families navigate these challenges, process their emotions, communicate effectively with each other and medical teams, and maintain their own wellbeing while supporting their loved one.
Collaborating with medical teams: Hospital psychologists function as integral members of healthcare teams, not isolated specialists addressing “mental health issues” separately from “real medicine.” They help physicians understand how psychological factors affect treatment adherence, pain management, and recovery. They facilitate difficult conversations about prognosis and treatment options. They identify when psychiatric symptoms require intervention. They contribute to discharge planning that accounts for psychological readiness, not just medical stability.
Consider someone receiving a diagnosis of terminal illness. The medical team provides crucial information about prognosis and treatment options, but processing this news requires more than medical facts. A hospital psychologist helps the patient work through initial shock, explore what matters most to them, communicate with loved ones, make decisions aligned with their values, and find meaning even as life’s horizon contracts. This psychological support doesn’t compete with medical care—it makes medical care more effective and more humane.
Transforming Patient Experience
The presence of hospital psychologists measurably improves patient outcomes and experiences. Research consistently demonstrates that addressing psychological needs enhances medical treatment effectiveness.
Psychological support reduces anxiety and depression, which commonly accompany serious illness. This matters not just for patient comfort but because depression and anxiety compromise immune function, increase pain perception, interfere with sleep and healing, and reduce treatment adherence. Addressing these psychological factors directly contributes to physical recovery.
Hospital psychologists improve treatment adherence—following medication regimens, attending appointments, making recommended lifestyle changes. When patients feel emotionally supported and their concerns are addressed, they engage more actively in their care. When psychological barriers to adherence are identified and addressed, medical treatments work better.
Pain management represents another area where psychology proves essential. Psychological factors profoundly influence pain experience. Anxiety amplifies pain, while effective coping strategies reduce it. Hospital psychologists teach techniques like relaxation, visualization, and cognitive reframing that complement medical pain management, often reducing medication needs.
Perhaps most importantly, psychological support helps patients maintain dignity and quality of life throughout treatment. Someone facing difficult medical circumstances still needs to feel seen as a person, not a diagnosis. They need space to express fears without being told to “stay positive.” They need help navigating relationships that shift under illness’s weight. They need support finding meaning when illness disrupts life plans.
Patients receiving integrated psychological and medical care consistently report better experiences, greater satisfaction, and improved quality of life—outcomes that matter enormously, regardless of medical prognosis.
Navigating Profound Challenges
Hospital psychology demands working with some of life’s most difficult realities. Hospital psychologists regularly encounter suffering that can’t be fixed, witness the impact of devastating diagnoses, support families making impossible decisions, and sit with people as they approach death.
Supporting critically ill patients requires emotional resilience. A psychologist might work with someone on a ventilator who can’t speak, using alternative communication to understand their fears and wishes. They might help someone come to terms with permanent disability, working through profound grief over lost capacities. They might support someone facing disfiguring surgery, addressing body image concerns and identity shifts.
Participating in delivering or processing bad news represents another challenging dimension. While physicians typically deliver diagnoses, hospital psychologists often support patients and families immediately afterward, helping them absorb devastating information and begin grappling with its implications.
Working with bereaved families requires holding space for overwhelming grief while also providing practical support with decisions about organ donation, autopsy consent, or simply leaving the hospital after loss. These moments demand profound empathy combined with clarity and steadiness.
Children’s hospitals present unique challenges. Helping children understand illness and treatment in developmentally appropriate ways, supporting them through painful procedures, addressing trauma from medical experiences, and helping families maintain as much normalcy as possible requires specialized skills and creativity. A psychologist might use play therapy to help a young child process what’s happening, create coping strategies through stories and games, or help siblings understand why their brother or sister is receiving so much attention.
Despite these challenges—or perhaps because of them—hospital psychology remains deeply meaningful work. Hospital psychologists know their presence matters profoundly during people’s most vulnerable moments. They witness both devastating losses and remarkable resilience. They contribute to care that honors human dignity even in clinical settings.
The Path to Hospital Psychology Practice
Becoming a hospital psychologist requires both foundational training and specialized preparation. After completing a psychology degree, aspiring hospital psychologists typically pursue specialized training through several possible paths.
Many complete formal specialization programs in health psychology or hospital psychology, gaining concentrated knowledge about medical systems, common psychological responses to illness, collaborative practice with medical teams, and ethical considerations in healthcare settings.
Multi-professional residency programs offered by many hospitals provide intensive, supervised clinical training. Residents work across hospital departments, developing expertise in diverse medical contexts while receiving mentorship from experienced hospital psychologists.
Beyond formal credentials, effective hospital psychology requires developing specific competencies. Deep empathy allows psychologists to connect with suffering patients and families. Active listening skills help them understand concerns that patients struggle to articulate. Emotional resilience enables them to engage repeatedly with difficult situations without burning out or becoming emotionally numb. Cultural competence ensures they can work respectfully with diverse populations. Medical knowledge helps them understand conditions, treatments, and prognoses well enough to address relevant psychological factors. Ethical sensitivity guides navigation of complex situations involving confidentiality, capacity, end-of-life decisions, and family dynamics.
Hospital psychologists also commit to ongoing professional development, staying current with research on health psychology, medical advances that create new psychological challenges, and evolving best practices for integrated care.
Humanizing Healthcare
At its core, hospital psychology represents healthcare’s commitment to treating whole people rather than isolated symptoms. It recognizes that healing involves more than fixing what’s broken in the body—it requires attending to the psychological and emotional dimensions of illness that profoundly affect both the experience of being ill and the process of recovery.
When hospital psychologists collaborate effectively with medical teams, something shifts. Patients feel seen and valued. Families feel supported through terrifying uncertainty. Medical staff gain insight into factors affecting their patients’ wellbeing beyond what appears on diagnostic tests. The entire hospital environment becomes more humane.
This doesn’t mean eliminating suffering—sometimes suffering is inherent to illness and treatment. But it means ensuring that no one suffers alone, that emotional needs receive the same careful attention as physical symptoms, and that even in the midst of serious illness, people maintain dignity, connection, and the opportunity to make meaning of their experience.
If you or someone you love faces hospitalization, knowing that psychological support is available—and that requesting it represents strength, not weakness—can make a profound difference. Hospital psychologists exist precisely to help patients and families navigate these challenging experiences with greater support, clarity, and compassion.
Medicine at its best treats the whole person. Hospital psychology ensures that this aspiration becomes reality.

