Can Psychologists Prescribe Medication? Understanding Professional Roles in Mental Healthcare
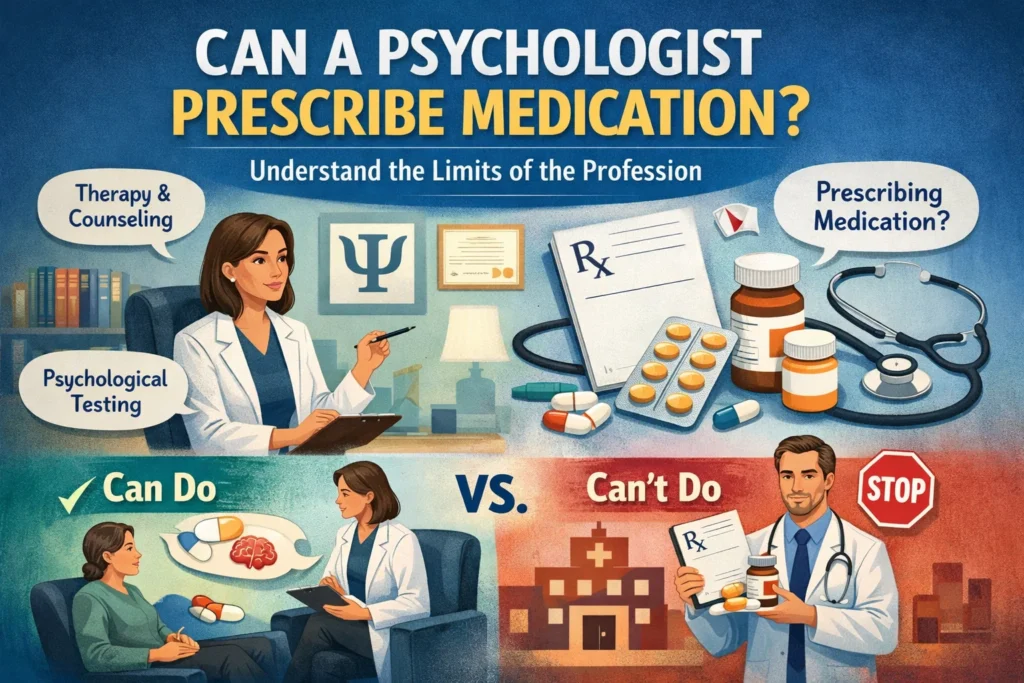
When facing emotional struggles or mental health challenges, many people wonder about the different types of help available and what each professional can offer. One common question arises repeatedly: “Can a psychologist prescribe medication?” Understanding the answer—and the reasons behind it—helps you navigate mental healthcare more effectively and know which professionals to consult for different needs.
The straightforward answer is that in Brazil, psychologists cannot legally prescribe medication. This limitation isn’t arbitrary but reflects fundamental differences in training, expertise, and professional roles. Far from diminishing psychology’s value, these distinctions clarify how different mental health professionals contribute uniquely to your wellbeing.
Why Psychologists Don’t Prescribe Medication
The legal framework governing psychology in Brazil, established by Law No. 4,119/1962, defines the scope of psychological practice. This legislation authorizes psychologists to conduct psychological assessment, provide psychotherapy, perform psychological testing, offer preventive interventions, and address emotional and behavioral concerns through psychological methods.
Notably absent from this scope is prescribing medication—an activity reserved for physicians and, in specific limited contexts, other healthcare professionals with particular medical training.
This distinction reflects the fundamental difference in how psychologists and physicians are educated. Medical training, including psychiatry, focuses extensively on human physiology, biochemistry, pharmacology, and the biological bases of disease. Physicians learn how medications interact with bodily systems, how to interpret laboratory results and physical examinations, how to monitor for side effects and drug interactions, and how to adjust dosages based on physiological responses.
Psychologists receive entirely different training. Their education emphasizes understanding human behavior, emotions, thoughts, relationships, and development. They learn therapeutic techniques for facilitating psychological change, assessment methods for understanding psychological functioning, research on what helps people overcome difficulties, and theories about how psychological problems develop and resolve.
These aren’t inferior skills—they’re different skills addressing different dimensions of mental health. Psychology and medicine approach mental wellbeing from complementary but distinct angles.
Consider someone experiencing depression. A psychiatrist examines whether biochemical factors might be contributing, assesses whether medication could help regulate neurotransmitter systems, monitors for medical conditions that can cause depressive symptoms, and prescribes medication when clinically indicated. A psychologist explores the thoughts, behaviors, relationships, and life circumstances contributing to depression, teaches coping strategies and skills, addresses underlying psychological patterns, and helps the person process difficult emotions and experiences.
Both approaches offer genuine value. Neither is complete without the other for many people struggling with mental health challenges.
What Psychologists Can Do Regarding Medication
While psychologists don’t prescribe medication, they play crucial roles in how clients navigate pharmacological treatment. Understanding these contributions clarifies how psychologists and prescribing professionals work together.
Recognizing when medication evaluation is needed: Psychologists are trained to identify signs and symptoms suggesting that psychiatric evaluation might benefit a client. When someone presents with symptoms that commonly respond well to medication—severe depression, debilitating anxiety, psychotic symptoms, bipolar disorder indicators, ADHD patterns—responsible psychologists recognize these presentations and recommend psychiatric consultation.
This referral isn’t an admission that therapy has failed. It’s professional recognition that the client might benefit from all available treatment options, including medication. Many conditions respond best to combined treatment—both medication and psychotherapy—rather than either alone.
Supporting clients through medication concerns: Starting psychiatric medication often triggers anxiety, uncertainty, and resistance. People worry about side effects, fear becoming dependent, feel stigma about needing medication, or believe taking medication means they’re “weak” or have failed somehow.
Psychologists can address these concerns therapeutically. They provide space to explore fears and ambivalence, offer accurate information to counter misconceptions, normalize the experience of needing medication, and work through the emotional meaning someone attaches to taking psychiatric drugs.
For instance, someone prescribed antidepressants might feel ashamed, believing they should be able to “just think more positively.” A psychologist can help them examine where this belief originates, challenge the stigma surrounding mental health treatment, and recognize that depression involves genuine physiological changes, not simply “bad attitudes” requiring more willpower.
Monitoring response and supporting adherence: Once clients begin medication, psychologists often notice changes before psychiatrists do, simply because therapy involves more frequent, longer contact. Psychologists can observe whether medication seems helpful, identify concerning side effects that warrant medical attention, notice if someone has stopped taking medication, and understand psychological barriers to consistent medication use.
This information helps psychiatrists make better treatment decisions. A psychologist might notice that a client stopped taking medication not because of side effects but because of shame about needing it—information that shifts how the psychiatrist approaches the conversation about adherence.
Maximizing medication effectiveness through therapy: Research consistently shows that for many conditions, particularly depression and anxiety disorders, combining medication with psychotherapy produces better outcomes than either treatment alone. Medication may reduce symptom intensity enough that psychological work becomes possible, while therapy addresses underlying patterns that medication alone doesn’t change.
A psychologist helps clients use the relief medication provides to engage more effectively in therapeutic work, developing skills and insights that support long-term wellbeing even after medication is eventually discontinued.
Psychologists and Psychiatrists: Complementary Expertise
Understanding the distinction between these professions helps you make informed decisions about your mental healthcare.
Psychiatrists are physicians who specialized in mental health after completing medical school. Their medical training allows them to diagnose mental disorders from a medical perspective, prescribe and manage psychiatric medications, order and interpret medical tests, identify medical conditions affecting mental health, and provide medical monitoring throughout treatment.
Psychiatry appointments often focus on symptom assessment, medication management, and monitoring treatment response. While some psychiatrists also provide psychotherapy, many focus primarily on pharmacological treatment due to time constraints and the medical complexity of psychiatric medication management.
Psychologists complete graduate training in psychology (typically a five-year degree in Brazil, often followed by specialization). Their education emphasizes psychological assessment using validated tests and interviews, various psychotherapy approaches (Cognitive Behavioral Therapy, psychoanalysis, humanistic therapy, systemic therapy, among others), understanding psychological development and functioning, and research on psychological interventions.
Psychology sessions typically involve deeper exploration of thoughts, feelings, relationships, and life patterns, along with developing new skills and perspectives that support psychological wellbeing.
These professionals often work together, creating comprehensive care that addresses both biological and psychological dimensions of mental health. Someone with an anxiety disorder might see a psychiatrist monthly for medication management while attending weekly therapy sessions with a psychologist to understand anxiety triggers, develop coping strategies, and address underlying fears or beliefs.
This collaborative approach recognizes that mental health involves both brain and mind, biology and psychology, medication and meaning-making. Neither professional alone provides everything most people need for comprehensive mental healthcare.
International Variations in Prescribing Authority
In a few U.S. states and territories—including New Mexico, Louisiana, Illinois, Iowa, and Idaho—psychologists can obtain limited prescribing privileges after completing extensive additional training in psychopharmacology, typically including a post-doctoral master’s degree in clinical psychopharmacology and supervised clinical hours.
This model, called prescriptive authority for psychologists, aims to increase access to mental healthcare, particularly in underserved areas where psychiatrists are scarce. Proponents argue that psychologists’ training in assessment and therapy, combined with pharmacology education, creates well-rounded providers. Critics worry about patient safety and believe medical training provides essential foundation for prescribing.
This remains controversial even in the United States, with most states maintaining the traditional division where psychologists provide therapy and physicians prescribe medication.
In Brazil, no such pathway currently exists. Brazilian legislation clearly reserves prescribing authority for physicians (and in very limited, specific contexts, other healthcare professionals like dentists prescribing within their scope). There’s no indication this will change in the foreseeable future.
Understanding this international variation clarifies that the question of who can prescribe isn’t about absolute truths but about how different countries structure their healthcare systems and professional roles.
Choosing the Right Professional for Your Needs
Knowing these distinctions helps you decide where to start when seeking mental health support.
Consider beginning with a psychologist if you’re experiencing:
- Emotional distress that’s affecting your daily life
- Relationship difficulties or family conflicts
- Grief, loss, or major life transitions
- Stress, worry, or general unhappiness
- Desire for personal growth or better self-understanding
- Behavioral patterns you want to change
- Trauma you need to process
Psychologists can address these concerns therapeutically and will recommend psychiatric consultation if medication appears beneficial.
Consider consulting a psychiatrist (or requesting a referral) if you’re experiencing:
- Severe symptoms significantly impairing functioning
- Suicidal thoughts or plans
- Psychotic symptoms (hallucinations, delusions)
- Extreme mood swings suggesting bipolar disorder
- Symptoms that haven’t improved with therapy alone
- Situations where you’re interested in exploring medication options
Often, the most effective approach involves both professionals working together, each contributing their distinct expertise to support your recovery and growth.
The Essential Value of Psychology
That psychologists can’t prescribe medication doesn’t diminish their profound importance in mental healthcare. If anything, their distinct focus creates space for the deep psychological work that medication alone can never provide.
Medication can be remarkably helpful—reducing symptom intensity, stabilizing mood, quieting intrusive thoughts, calming overwhelming anxiety. But medication doesn’t teach coping skills, resolve relationship conflicts, heal trauma, change problematic thought patterns, or help you understand yourself more deeply. These require psychological work that trained therapists facilitate.
Many people benefit enormously from therapy without ever needing medication. Others find medication essential but insufficient without the psychological growth therapy enables. The most common scenario involves needing both—each addressing different but equally important dimensions of mental health.
Understanding professional roles and limitations helps you access the full range of support available. When psychologists recognize medication might help and refer you to a psychiatrist, that’s professional integrity, not failure. When psychiatrists recommend therapy alongside medication, that’s comprehensive care, not doubt about their prescriptions.
Mental health challenges deserve responses as multifaceted as their causes. Psychology’s contribution to that comprehensive response remains absolutely essential, prescribing authority or not.
If you’re struggling and unsure where to start, choosing either a psychologist or psychiatrist begins the process. Whichever you choose, competent professionals will help you access additional support if needed, ensuring you receive care addressing all dimensions of your wellbeing.

