When to Seek a Psychologist: 7 Key Signs and What They Mean
One of the most common questions people ask themselves is: “Do I actually need therapy, or am I overreacting?” This uncertainty keeps countless people suffering unnecessarily, waiting for problems to become severe enough to justify seeking help. The truth is, you don’t need to be in crisis to benefit from therapy—and waiting until you are often makes recovery harder and longer.
Understanding when psychological support could help isn’t about pathologizing normal human experiences or suggesting everyone needs therapy. It’s about recognizing when struggles have crossed from temporary difficulty into patterns that diminish your quality of life, when your coping strategies aren’t working, or when professional guidance could help you navigate challenges more effectively.
This guide explores seven key indicators that therapy could be beneficial, what each sign means, and how to trust your judgment about seeking help.
Understanding When Professional Help Makes Sense
Before diving into specific signs, it’s important to understand what seeking a psychologist actually means and dispel some common misconceptions that prevent people from getting help.
Therapy Isn’t Just for Crisis
One of the most persistent myths about therapy is that it’s only for people in severe crisis—those who can’t function, are suicidal, or have diagnosed mental illnesses. This misconception causes people to minimize their own suffering: “Other people have it worse” or “I’m managing okay, so I don’t really need help.”
In reality, therapy serves multiple purposes beyond crisis intervention. It helps you develop self-awareness and emotional intelligence, navigate life transitions and difficult decisions, improve relationships and communication, process past experiences that affect current functioning, build coping skills before stress becomes overwhelming, and achieve personal growth and life satisfaction.
Waiting until you’re in crisis is like waiting until you can’t walk to address knee pain—technically possible, but it means enduring unnecessary suffering and facing a longer, harder recovery.
Prevention Is Powerful
Some of therapy’s most valuable work happens when people seek help before problems become severe. Early intervention prevents small difficulties from becoming entrenched patterns, addresses issues while you still have resources and resilience, and teaches skills that serve you throughout life.
Think of therapy like any other form of health maintenance. You don’t wait until you have advanced disease before seeing a doctor. You engage in preventive care—regular checkups, addressing concerning symptoms early, building healthy habits. Mental health deserves the same proactive approach.
The Courage in Seeking Help
Despite progress in mental health awareness, stigma still makes many people reluctant to seek therapy. They worry that needing help means they’re weak, broken, or incapable of handling their own problems. This couldn’t be further from the truth.
Seeking therapy demonstrates self-awareness (recognizing something isn’t working), emotional intelligence (understanding when you need support), problem-solving ability (taking action rather than suffering passively), and self-compassion (treating yourself with the care you deserve).
These are strengths, not weaknesses. The people who seek help are often more emotionally mature and self-aware than those who insist on struggling alone out of pride or fear.
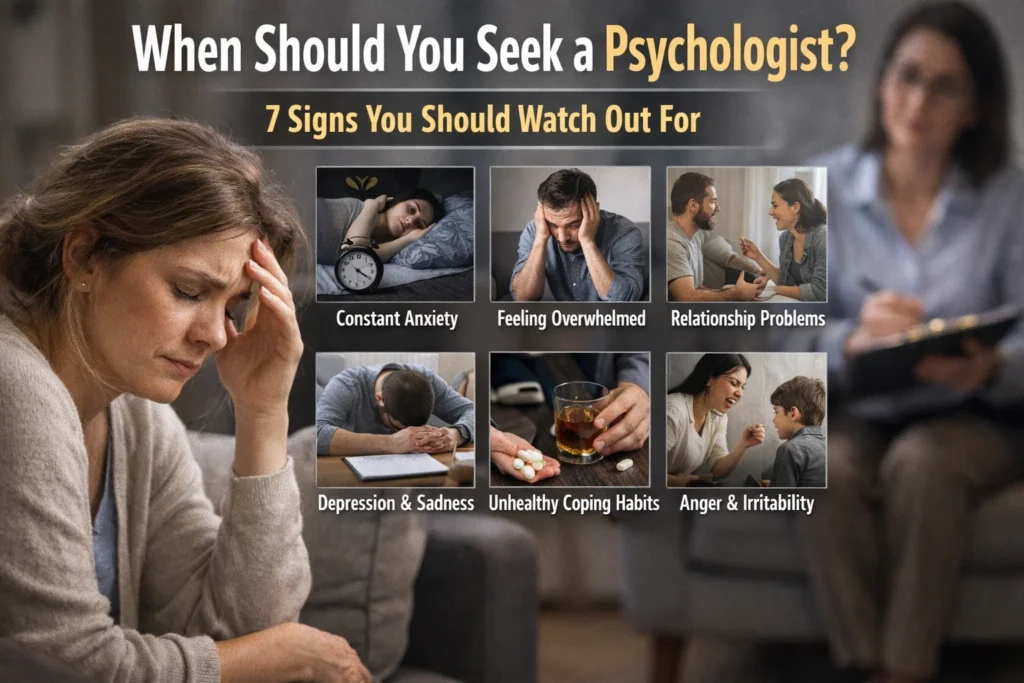
Seven Key Signs You Could Benefit from Therapy
While no checklist can definitively determine whether you need therapy, certain signs suggest that professional support could significantly improve your well-being. You don’t need to experience all of these—even one persistent sign might warrant reaching out.
1. Overwhelming or Persistent Difficult Emotions
Everyone experiences sadness, anxiety, anger, fear, and other difficult emotions. These are normal parts of being human. But when these emotions become overwhelming in intensity, persistent in duration (lasting weeks or months), disproportionate to circumstances, or significantly impair your functioning, they suggest something beyond normal emotional fluctuation.
What this looks like in practice:
You feel sad or empty most days for weeks, without clear improvement. Anxiety pervades your day, making routine activities feel overwhelming. Anger feels constantly near the surface, erupting over minor frustrations. Fear or worry feel uncontrollable, dominating your thoughts even when you recognize the concerns are disproportionate.
The key distinction is persistence and impact. A few days of sadness after disappointment is normal. Weeks of pervasive sadness that colors everything despite positive events suggests depression. Anxiety before an important presentation is normal. Daily, uncontrollable worry that prevents you from functioning suggests an anxiety disorder.
Why therapy helps:
A psychologist can help you understand what’s driving these emotions, develop strategies for managing them more effectively, identify and change thought patterns that intensify emotions, and determine whether you might benefit from additional interventions like medication.
2. Difficulty Coping with Loss, Trauma, or Major Life Changes
Certain experiences—death of loved ones, relationship endings, job loss, health diagnoses, traumatic events, or significant life transitions—profoundly impact emotional well-being. Struggling with these experiences doesn’t mean weakness; it means you’re human.
What this looks like in practice:
Grief that feels stuck rather than gradually processing. Trauma symptoms like flashbacks, nightmares, or hypervigilance that don’t improve with time. Inability to move forward after a major loss or change. Physical or emotional symptoms that appeared after a specific event. Avoidance of people, places, or activities connected to loss or trauma.
While grief and adjustment to change are normal, certain signs suggest you could benefit from support: symptoms that worsen rather than gradually improve, significant functional impairment lasting months after the event, using unhealthy coping mechanisms (substance use, self-harm, extreme isolation), or feeling stuck in ways that prevent healing.
Why therapy helps:
Psychologists are trained in grief counseling, trauma processing, and helping people navigate major transitions. They provide structured support for working through difficult experiences, offer proven techniques for processing trauma, help you develop healthy coping strategies, and create space to honor your experience while moving toward healing.
3. Relationship Patterns That Cause Suffering
Relationships—with partners, family, friends, or colleagues—significantly impact well-being. When relationship difficulties become patterns rather than isolated conflicts, therapy can help identify what’s going wrong and develop healthier ways of relating.
What this looks like in practice:
Repeatedly entering similar dysfunctional relationship patterns (choosing unavailable partners, attracting people who hurt you, experiencing the same conflicts in different relationships). Difficulty maintaining close relationships or forming meaningful connections. Communication problems that create misunderstanding and conflict. Inability to set or maintain boundaries. Extreme conflict in multiple important relationships. Isolation due to relationship difficulties or social anxiety.
One difficult relationship might reflect the other person’s issues. A pattern across multiple relationships suggests something in how you relate, communicate, or choose partners might benefit from exploration.
Why therapy helps:
Relationship patterns often have roots in early experiences, attachment styles, and learned communication habits. A psychologist can help you understand these patterns, recognize how past experiences influence current relationships, develop healthier communication and boundary-setting skills, work through fears of intimacy or abandonment, and build more satisfying, secure relationships.
4. Persistent Low Self-Esteem and Harsh Self-Criticism
Everyone experiences occasional self-doubt or self-criticism. But when negative self-perception becomes your baseline—when you fundamentally believe you’re inadequate, unworthy, or fundamentally flawed—it affects every aspect of life.
What this looks like in practice:
Constant internal criticism that you’d never direct at others. Difficulty accepting compliments or recognizing your strengths. Feeling you don’t deserve good things or happiness. Comparing yourself unfavorably to others constantly. Perfectionism driven by fear of being “not good enough.” Making yourself small to avoid judgment or rejection. Staying in situations that hurt you because you don’t believe you deserve better.
Low self-esteem isn’t just unpleasant—it influences decisions, limits opportunities, affects relationships, and can contribute to depression and anxiety.
Why therapy helps:
Self-esteem issues often develop from early experiences, repeated criticism, trauma, or distorted thinking patterns. Therapy helps you identify origins of negative self-beliefs, challenge distorted thinking about yourself, develop self-compassion and realistic self-assessment, recognize and internalize your actual strengths and value, and gradually build a healthier relationship with yourself.
5. Engaging in Self-Destructive or Risky Behaviors
When emotional pain becomes overwhelming, some people develop unhealthy coping mechanisms. These behaviors provide temporary relief or numbness but create additional problems and often indicate underlying issues requiring professional support.
What this looks like in practice:
Substance abuse—using alcohol or drugs to cope with emotions, escape reality, or numb pain. Self-harm behaviors like cutting, burning, or other intentional injury. Disordered eating—restrictive eating, binge eating, purging, or using food to manage emotions. Reckless behaviors that put you in danger—dangerous driving, unsafe sexual practices, unnecessary risk-taking. Compulsive behaviors that interfere with functioning—excessive gambling, shopping, internet use, or other compulsions.
These behaviors often serve a function—managing unbearable emotions, gaining a sense of control, punishing yourself, or feeling something when emotionally numb. Understanding the function helps develop healthier alternatives.
Why therapy helps:
Addressing self-destructive behaviors requires understanding what drives them and developing healthier coping strategies. A psychologist can help you identify emotional needs these behaviors address, develop alternative coping mechanisms, process underlying pain or trauma driving the behaviors, and create safety plans for managing urges.
For some self-destructive behaviors, specialized treatment approaches like dialectical behavior therapy (DBT) or intensive outpatient programs may be recommended.
6. Difficulty with Concentration, Decision-Making, or Daily Functioning
When your mind feels constantly foggy, when simple decisions feel paralyzing, or when tasks that were once routine now feel overwhelming, something beyond normal stress may be occurring.
What this looks like in practice:
Inability to focus on tasks that require concentration. Mind constantly wandering or feeling scattered. Simple decisions—what to eat, what to wear—feel overwhelming or impossible. Procrastination on important tasks due to anxiety or lack of motivation. Declining performance at work or school despite effort. Forgetting appointments, missing deadlines, or neglecting responsibilities. Executive function problems—difficulty planning, organizing, or completing tasks.
These cognitive symptoms often accompany depression, anxiety, ADHD, or high stress. They significantly impact functioning and quality of life, making it harder to meet responsibilities or pursue goals.
Why therapy helps:
Cognitive difficulties can result from various causes, and therapy helps identify the source—whether depression, anxiety, attention disorders, trauma, or stress—and address it. Therapy provides strategies for improving focus and organization, techniques for managing decision anxiety, support for addressing underlying conditions affecting cognition, and help developing systems that support functioning despite difficulties.
7. Physical Symptoms Without Clear Medical Cause
The mind-body connection means psychological distress often manifests physically. When doctors rule out medical causes for persistent physical symptoms, emotional or psychological factors may be responsible.
What this looks like in practice:
Chronic headaches or migraines without identified cause. Persistent digestive issues—stomach pain, nausea, irritable bowel symptoms. Chest tightness, heart palpitations, or shortness of breath not explained by heart or lung conditions. Chronic muscle tension, back pain, or body aches. Sleep disturbances—insomnia or hypersomnia. Chronic fatigue unrelieved by rest. Symptoms that worsen during stress or appear before anxiety-provoking situations.
These symptoms are real—not “all in your head” in the dismissive sense. Stress, anxiety, and depression create physiological changes affecting pain perception, inflammation, digestion, and more. The psychological origin doesn’t make them less legitimate.
Why therapy helps:
Addressing the psychological factors contributing to physical symptoms can provide significant relief. Therapy helps you learn stress management and relaxation techniques, understand mind-body connections, address anxiety or depression contributing to symptoms, and develop coping strategies that reduce physiological stress responses.
This works best in collaboration with medical providers who’ve ruled out physical causes and recognize the mind-body connection.
Additional Considerations: When Therapy Makes Sense
Beyond these seven key signs, other situations suggest therapy could be beneficial:
Life transitions, even positive ones, can benefit from therapeutic support—starting college, career changes, becoming a parent, retirement, or relocation. These transitions involve identity shifts and adjustment that therapy can help navigate.
Personal growth and self-understanding, even without specific problems. Some people seek therapy to better understand themselves, explore patterns, develop emotional intelligence, or work toward becoming the person they want to be.
Preventive support when you know you’re entering a challenging period—anticipating a difficult conversation, preparing for a stressful event, or building resilience before expected challenges.
When people who care about you express concern about changes they’ve noticed. While only you can decide if therapy is right, trusted people’s observations deserve consideration.
When you’re simply not happy with your life, relationships, or yourself, even if you can’t identify a specific “problem.” Therapy isn’t just for fixing problems—it’s for building a more satisfying life.
Trusting Your Judgment
Ultimately, you’re the expert on your own experience. If you’re wondering whether you need therapy, that wondering itself suggests you might benefit from it. The question “Do I need help?” rarely arises when everything is truly fine.
Trust your internal sense that something isn’t right, that you’re struggling more than you should be, that life could be better, or that you deserve support. You don’t need permission or a severe enough problem. If you’re suffering, if your quality of life has diminished, if you want things to be different—those are sufficient reasons.
Overcoming Barriers to Seeking Help
Even when people recognize they could benefit from therapy, common barriers prevent them from reaching out:
“I should be able to handle this myself.” Seeking help isn’t weakness or failure—it’s using available resources to address challenges, just as you’d see a doctor for physical problems or hire an accountant for complex finances.
“Other people have it worse.” Your suffering doesn’t require comparison to others’ struggles to be valid. You deserve support regardless of whether someone somewhere has bigger problems.
“I can’t afford therapy.” Many psychologists offer sliding-scale fees based on income. Community mental health centers, university training clinics, and some nonprofits provide low-cost or free services. Employee assistance programs often include free therapy sessions. Online therapy platforms are typically less expensive than traditional therapy.
“I don’t have time.” Therapy typically requires one hour weekly—less time than many people spend on social media daily. Consider it an investment in yourself that makes the rest of your time more productive and satisfying.
“What will people think?” Therapy is confidential. You’re not required to tell anyone. But increasingly, people recognize seeking therapy as healthy and responsible rather than shameful.
“What if therapy doesn’t help?” Most people who engage fully in therapy experience significant benefit. If the first therapist isn’t a good fit or approach doesn’t help, you can try different therapists or approaches. Not trying means guaranteed continued suffering.
Taking the First Step
If you recognize yourself in these signs, consider reaching out to a psychologist for an initial consultation. This doesn’t commit you to long-term therapy—it’s simply an opportunity to explore whether professional support could help.
Look for psychologists through your insurance provider’s network, professional psychology association referral services, recommendations from your doctor or trusted friends, or online therapist directories that allow searching by specialty and approach.
When you contact potential therapists, it’s appropriate to ask about their experience with concerns like yours, their therapeutic approach, practical details like fees and scheduling, and whether they offer initial consultations to assess fit.
Many people spend weeks or months considering therapy before making that first call. If you’ve been thinking about it, that’s a sign it’s time to reach out. The anticipation is often worse than the reality, and starting therapy is often followed by relief at finally taking action and regret about not doing it sooner.
Moving Forward
Recognizing you could benefit from therapy is the first step. Taking action on that recognition is the second. Between those two steps, many people get stuck—knowing they should seek help but not quite doing it, waiting for the “right time,” hoping things will improve on their own, or letting fear and uncertainty win.
If you’ve read this far, you’re probably past the “should I?” question and into the “when will I?” phase. The answer is: now is as good a time as any. Problems rarely resolve themselves through waiting, and the sooner you start, the sooner you begin feeling better.
You deserve support. You deserve to feel better. You deserve a life not dominated by suffering, difficult emotions, or limiting patterns. Therapy offers a path toward that better life—not a perfect life free of challenges, but one where you have the tools, understanding, and resilience to navigate whatever comes with greater ease and satisfaction.
That first phone call might feel daunting, but it’s also the beginning of taking your mental health seriously, investing in your well-being, and giving yourself the support you deserve. The hardest step is the first one. After that, you’re no longer facing your struggles alone.
Ready to learn more about therapy and mental health? Explore our related articles: Your First Therapy Session: What to Expect | How Psychotherapy Transforms Anxiety | 14 Warning Signs of Depression

